Clinical conditions of children with disability have been changing as medical technology progressed. Before, children with the most severe disability were those who are unable to leave bed and speak. But with better medical technology, more children are saved. This led to the appearance of children who are not only unable to leave bed or speak, but also dependent on medical devices and care such as tube feeding, tracheotomy, and ventilators.
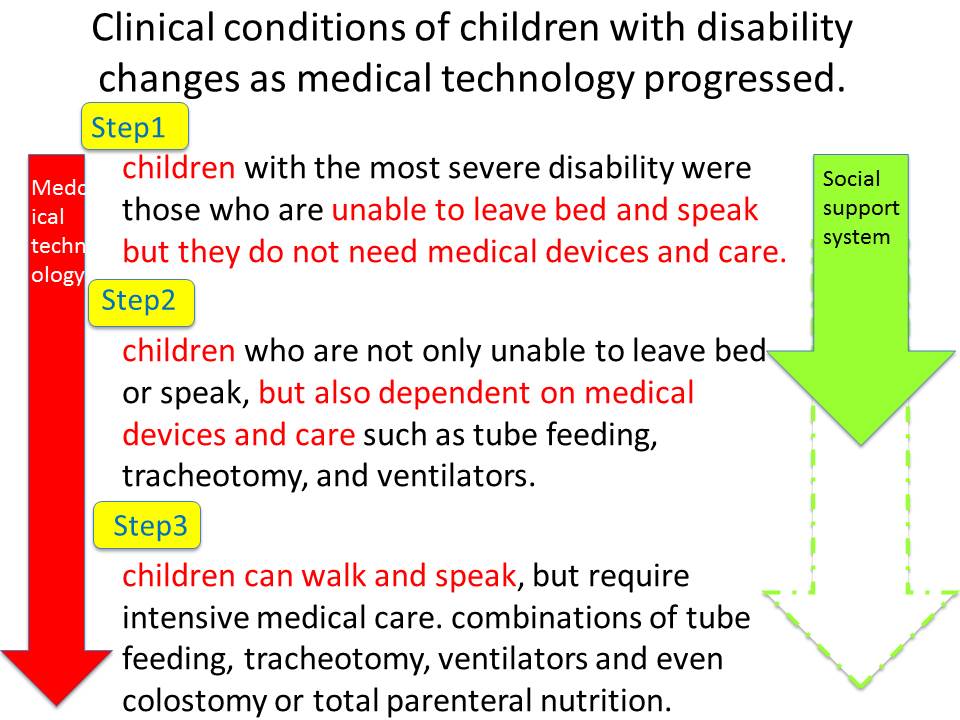
With further advancement of medical technology, we can now save children who are born with very complicated congenital heart disease or other congenital diseases that cause abnormality in esophagus or trachea. These children can walk and speak, but require intensive medical care. They need combinations of tube feeding, tracheotomy, and ventilators. Some even require colostomy or total parenteral nutrition. However, in Japan Children who can’t walk or speak with complex disabilities are regarded as a template target of the welfare service for the disabled. Because medical devices and cares are not considered, the service does not cover children who can walk and speak by law. In reality, there is some flexibility in the system, and so it is not completely useless, but it is clear that our social system is not catching up with the way the clinical conditions of these children have changed. This is an example where the speed of medical technology advancement far exceeded that of social system.
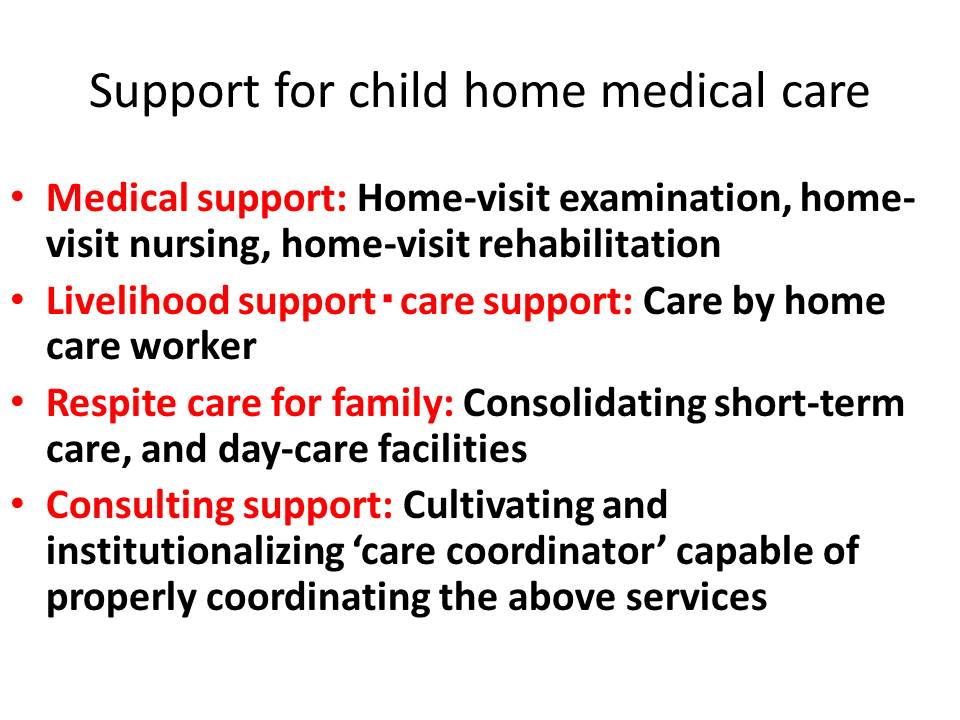
Regarding pediatric home care support, medical care, life support and respite care are critical or indispensable. Also, effectively combining these factors require consultation and coordination functions.
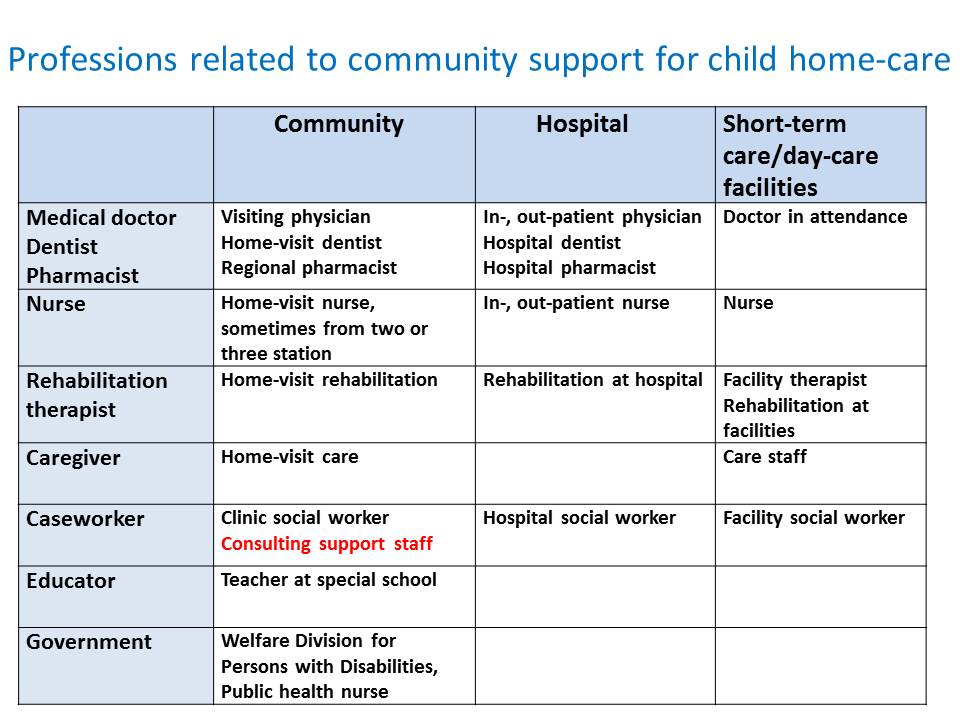
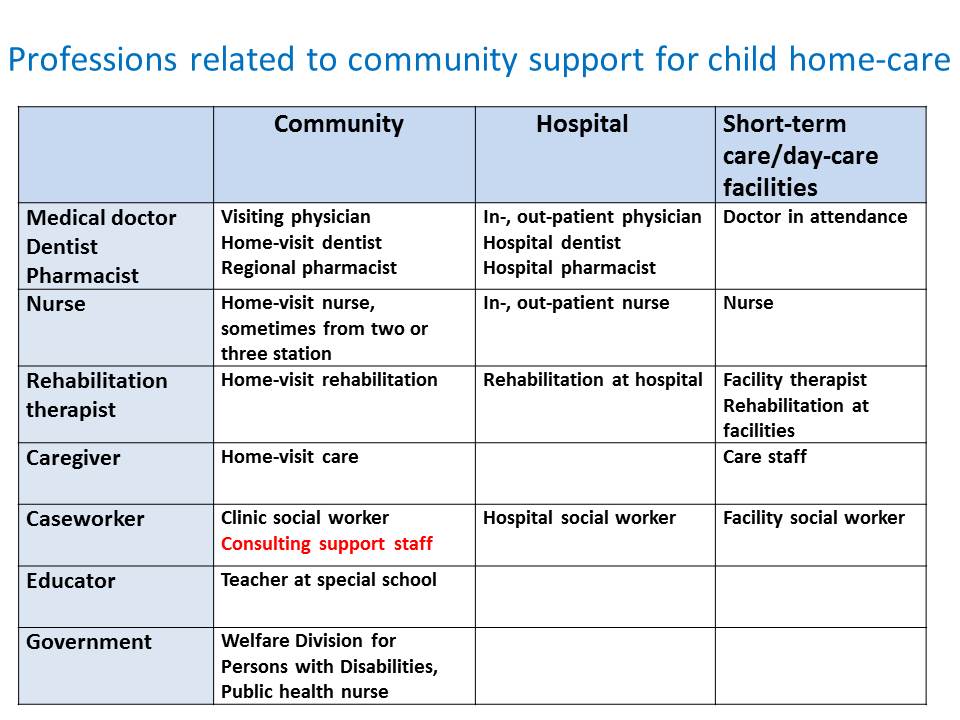
As shown here, we need various professions to provide pediatric home care.
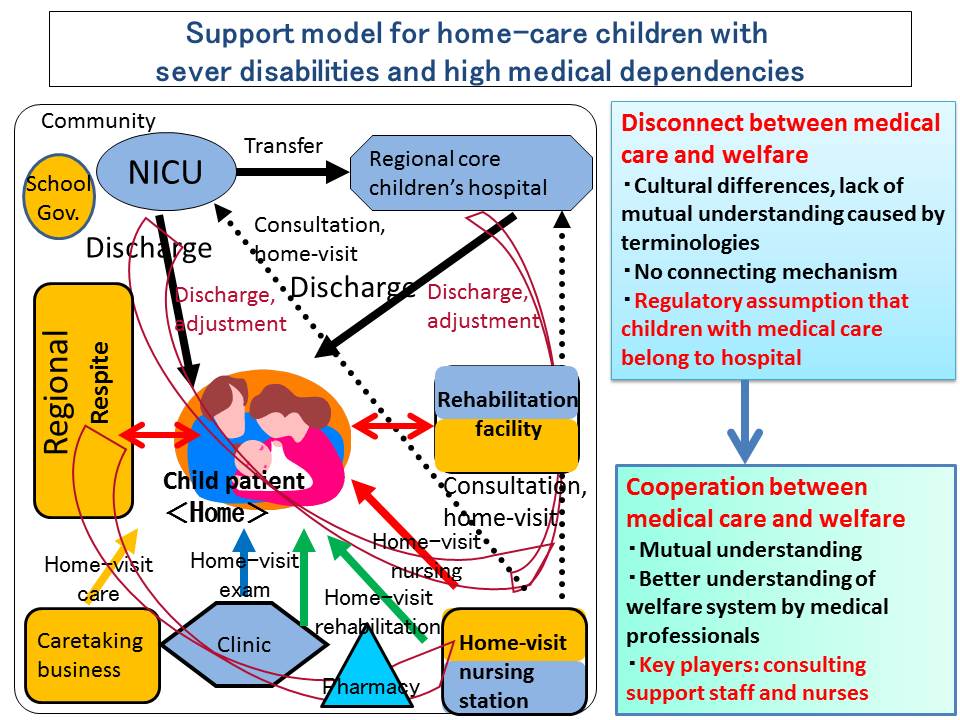
This includes medical, welfare, education, and government. But there is no proper system to connect these functions. In particular, the gap between medical care and welfare is so huge that we don’t even notice it exists. The cultures and the languages in these two functions are completely different. The difference in technical terms makes communication difficult. That is, because the system of child welfare wasn’t created with the idea that children who need medical devices and care live in local communities. The situation has changed drastically just in the last a few decades, so the system couldn’t catch up. Just two decades ago, the case of a child with ventilation living in a local community is an exception. There was no need to build the system for such a rare case and we are still in that mindset. We need to overcome this hurdle, begin to understand each other between medical and welfare, and collaborate to support children.
This slide shows the profession related to pediatric in-home medical care. doctors, dentists, pharmacists, nurses, rehabilitation therapists, caseworkers, educators and government officers are listed. I listed community, hospital, short-stay and day-care facilities as the main workplace for each profession. In hospitals, in most cases, we have different doctors in outpatient and inpatient departments. Besides, we have additional doctors in respite care and short-stay facilities. (Most of them are facilities for severely disabled children or national hospitals.)
You will see its complexity if you compare it to the nursing-care insurance system for the elderly.
For the elderly, we have less number of professions involved in the system. We have care managers as coordinators. For doctors, as I mentioned earlier, it is rare that the doctor at a hospital keeps taking care of patients after discharge. That is, because initially the target of the medical in-home care is those who have difficulty in going hospital. Thus, a primary doctor in this case is a home visiting doctor. The role of hospital doctors will be limited to performing intensive inpatient therapy such as infection care.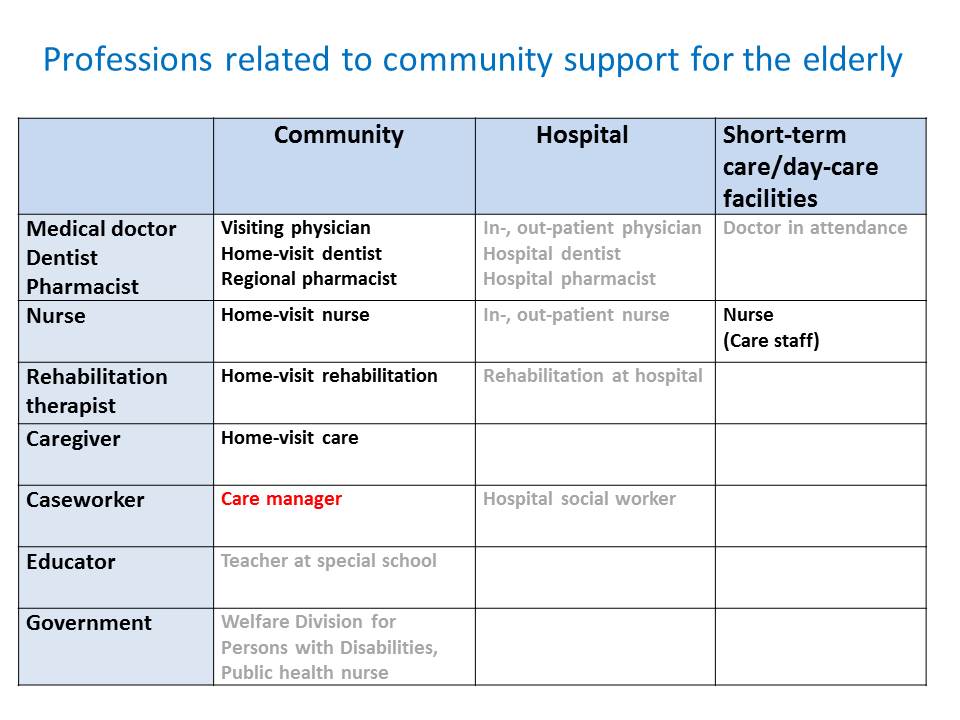
But as I mentioned earlier, in the case of children, most of them keep visiting out-patient hospital. In addition, hospital doctors often play a key role in deciding the direction of the therapy and home care doctors play a supportive role. The role that the home care doctors play is often different from that in adult home care. Therefore, collaboration between the doctors becomes important. But collaboration is usually difficult because of the differences in working environment.